A major expansion of services provided by high street pharmacies grabbed the headlines when NHS England announced its new blueprint to improve access to primary care. But just as significant in our view was the weight given to remote care.
The delivery plan stated: “Home monitoring can substantially improve health outcomes and reduce the need for regular and urgent appointments. A good example is blood pressure control through home monitoring, reducing heart attacks and strokes. To make home monitoring easier for patients and practices, we are funding the digital tools for patients to send their readings to their practice, where staff can review and add them to their clinical record with one click.”
High blood pressure accounts for more than one in 10 GP visits and treating it costs the NHS £2 billion a year, according to the National Institute for Health and Care Research. In Scotland, there are more than one million GP appointments every year just to measure blood pressure.
Inhealthcare has partnered with the NHS in Scotland to launch one of the biggest remote monitoring services for blood pressure to date. At the time of writing, nearly 6,000 patients have benefited from the national programme in Scotland.
In southern England, Inhealthcare has partnered with Surrey Heartlands, an integrated care system, to provide remote care to patients with high blood pressure. An NHS evaluation has illustrated how the approach is enhancing long-term condition management.
Of the 2,100 patients from high-risk cohorts who engaged with the service between October 2021 and December 2022, nearly half are now being treated to target. This means they are providing green category readings for both systolic and diastolic blood pressure.
To quote GP Richard Wright, clinical director for North Tandridge Primary Care Network: “The workload of managing high blood pressure that used to fall on GPs and practice nurses has very much been taken over…
“As a GP, there’s a sense we have a greater degree of confidence in the way this cohort is being managed. It’s a good level of supervision they are being managed with, and the way the monitoring occurs using the traffic light system provides a great deal of reassurance.”
NHS England’s plan promises to improve access to care, better support patients to manage their own health and modernise general practice for future generations. Much of the reaction focused on the expansion of high street pharmacy services, including providing medication for common conditions for the first time, which is clearly a radical step forward.
We believe remote patient monitoring has significant untapped potential to create extra capacity within primary care services. Consider the following calculations:
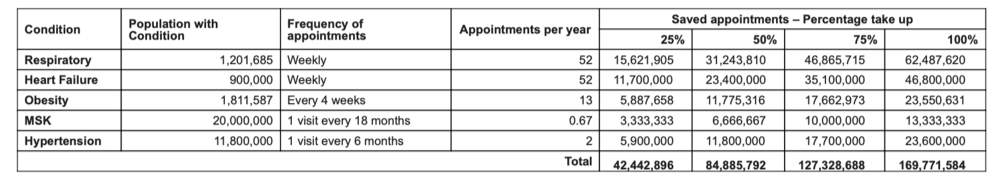
Even in the lowest take-up scenario, NHS England would still be looking at 42 million-plus saved appointments per year. Given that general practice currently delivers an estimated 300 million consultations per year, according to NHS England, this could be a game-changer for the patient and the public purse and truly open up access to primary care.

